Trusted data: The key to improved patient experiences
Enhancing patients’ healthcare experiences is more than just providing top-notch clinical care to improve outcomes—it’s a business necessity. McKinsey research shows that providers focused on improving the patient experience saw revenues increase by up to 20 percent over five years, while costs to serve decreased by up to 30 percent. One of the reasons is that satisfied patients are 28 percent less likely to switch providers.
The good news is that better patient experiences are also associated with lower medical malpractice risk, as well as greater employee satisfaction, leading to lower turnover. Patients with better care experiences often have better health outcomes—an important factor as the industry moves towards value-based care models, reimbursing providers for the quality—not quantity—of services.
In our blog posts, we have talked about the importance of having a trusted data foundation to deliver superior customer experiences. Healthcare is no exception. As healthcare providers invest in digital channels and analytics, the need for improving data quality and trust in the core business data takes a higher priority.
High-quality, trusted data provides the foundation for seamless patient experiences
In this blog post, I want to walk you through a few key elements that define the patient experience and the critical role high-quality, trusted data plays.
Care interactions: As patients play an increasing role in their own care, you need to deliver personalized, consistent experiences across all patient touchpoints. So your patients can easily search for a physician online, schedule their appointments, and communicate with care teams—and view their test results and other information on your portal, and via smartphone alerts and reminders. If you have fragmented, poor-quality patient and provider data, you probably can’t deliver consistent patient interactions at those touchpoints.
Care continuity: Your care teams need a comprehensive view of health history and speed up diagnosis to optimize care. But due to separate EHR and other systems used by various organizations across the care continuum—each with their own data quality challenges—it can be difficult for your teams to get a complete view and trust the data in front of them. Reliable patient data linking is crucial to building accurate longitudinal patient records with clinical histories to support decision-making and better health outcomes.
Care compliance: One way to improve patient outcomes is to help your patients follow doctors’ orders after appointments or hospital discharges. You also want to encourage them to make healthy choices and advise them when to seek help. However, poor quality patient data, such as inaccurate contact data and communication preferences, makes it harder for you to communicate with the patients and their care providers at their homes. This impedes your efforts to deliver care and guidance to them in a timely and compassionate manner.
Denied claims: According to reports, average claim denial rates are between 6% and 13%—and trends show denial rates are increasing. This frustrates patients by creating extra work to chase down providers and payers to understand the reason behind denied claims. And it frustrates your staff and slows your claims reimbursements. You can minimize these denials by reducing errors through consistent and accurate patient, physician, location, and other data in your systems.
Specialty referrals: Inaccurate provider directories block patients’ efforts to find the right physician—in-network, near home, and with the right specialty. It not only creates a poor patient experience, but it also leads to patients choosing a physician in a different provider network. One study compared Medicare’s database with physician directories, and only 19% of directories had consistent address and specialty information. An accurate provider directory should also be able to integrate third-party data ensuring referrals are timely and accurate, which increases patient satisfaction and loyalty. Research shows that with accurate provider data, this referral leakage can be reduced significantly and could even boost your revenue by as much as 10 to 30 percent.
Surprise bills: Erroneous directories not only make it difficult for patients to find an in-network provider near their home, but it also can result in some not obtaining timely care or paying too much for it (“surprise bills”). And with the No Surprises Act, you can incur additional costs and fines when a patient inadvertently receives out-of-network care due to bad provider directory information.
All these areas are positively impacted by having clean, unified, and trusted data available when you and your patients need it.
How modern master data management (MDM) improves patient experiences
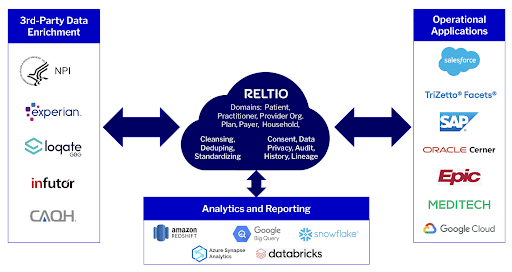
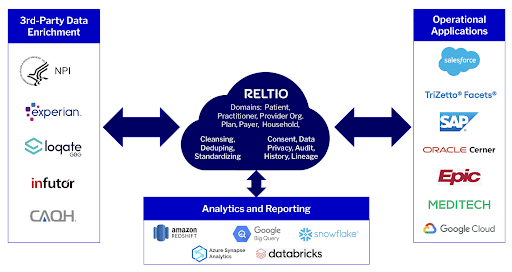
Modern MDM unifies and cleanses your core data, reliably links patient profiles from across systems, enriches it with third-party data, and delivers it in real time where it is needed. This trusted data fuels your operational and analytics systems, and gives you an accurate view into relationships with the patient across all data sources. You gain visibility into patient interactions across all channels including, doctor’s appointments, hospital visits, insurance claims, post-op follow-ups, and more.
Having consistent, trusted data enables you to:
- Enhance patient experiences across all touchpoints, streamlining their interactions with your organization
- Improve patient health outcomes by improving continuity of care, care compliance, and patient analytics
- Decrease patient spending by reducing claims denials and helping them avoid surprise bills
- Make it easier for patients to find the right referrals, which also reduces your revenue leakage
Reltio for Healthcare: Faster time-to-value and lower IT costs
We introduced the first cloud-native, SaaS MDM, which unified—in real time—core data from multiple sources into a single source of trusted information. And now we raised the bar one more time with our Reltio for Healthcare velocity pack to reduce your MDM implementation time to weeks.
Our velocity pack provides:
- An out-of-the-box healthcare data model with patients (and their households), practitioners, HCOs, health plans, and payers, which you can use as is or extend as needed
- Predefined configurations—driven by best practices—for cleansing, matching, survivorship, and UI
- Provisioned NPI integration for data enrichment
- Prescriptive implementation methodology
In addition, we integrate with Google Cloud Healthcare Data Engine to make it easier for you to build longitudinal patient records with trusted data for advanced analytics and operational decisions.
We also provide a healthcare business-value framework to help you prioritize use cases and expand the value over time. Overall, we help you implement a simplified, agile, and cost-effective MDM fast, so you can start delivering better patient experiences and health outcomes sooner.
We are excited to be part of healthcare’s patient experience transformation by providing an innovative way to quickly implement MDM tailored for your industry. So instead of worrying about getting the right data, you can focus on delivering the best patient experiences and health outcomes.
The impact of modern data management is not limited to patient experience. Operational efficiency—gained in both data operations and business processes—reduces cost, lowers risk, and improves compliance. Watch for our next blog on how trusted data can help you improve operational metrics, streamline payer interactions, and simplify compliance. To dive deeper into the velocity pack and the platform capabilities, you can reach out to our experts for a customized demo.
